Month: April 2023
Connie Francis – My Heart Has a Mind of Its Own
Ernest Tubb – Games People Play
Billy Strings – War Pigs
MOUNTAIN – Mississippi Queen
According to Sergeant Major Supro.
This thundering version of Mississippi Queen, Live in the studio at WITF Pennsylvania, USA shows the band at their peak power. They are sufficiently stimulated for the experience and giving it their all (except the keyboard player, wtf). This version is much better than the album version and the live version at NY Pop later in 1970, and is undoubtedly the best version of the song anywhere. This is the Holy Grail of MOUNTAIN relics.
Bob Dylan – Visions Of Johanna
According to FAR OUT MAGAZINE.
Ranking the songs on Bob Dylan’s masterpiece ‘Blonde on Blonde’. Worst to Best…
14. ‘Pledging My Time’
13. ‘Absolutely Sweet Marie’
12. ‘Obviously Five Believers’
11. ‘Temporarily Like Achilles’
10. ‘One of Must Know (Sooner or Later)’
9. ‘Fourth Time Around’
8. ‘Most Likely You Go Your Way (And I’ll Go Mine)’
7. ‘Leopard-Skin Pill-Box Hat’
6. ‘Rainy Day Woman #12 & 35’
5. ‘Sad-Eyed Lady of the Lowlands’
4. ‘I Want You’
3. ‘Stuck Inside of Mobile with the Memphis Blues Again’
2. ‘Visions of Johanna’
1. ‘Just Like A Woman’
Grateful Dead – Visions of Johanna
Little Richard – California I’m Comin
Jimmie Rodgers – Blue Yodel No. 4
Howlin’ Wolf – California Blues
Grateful Dead – Estimated Prophet
ANGELS AND DEMONS: THE PECULIAR AND HAUNTED GENIUS OF DR. HALSTED

A Johns Hopkins founding physician, William Stewart Halsted, with the help of his wife, Caroline Hampton, pioneered modern surgery as he waged a lifelong battle against drug addiction. One hundred years after his death, his legacy continues.
Katie Pearce / PublishedFall 2022
In the logbooks of the Butler Hospital for the Insane, there appears in May 1886 the feeble signature of a “William Stewart.” Like most patients at the Rhode Island hospital, the 33-year-old did not enter of his own volition but at the insistence of loved ones who witnessed his dark unraveling.
William Stewart Halsted—his full name, which he was presumably too ashamed to sign—may have been the most promising surgeon in America at that time. For six years, rotating among six different hospitals in New York City and teaching sought-after classes at night, he had been transforming the field from one of rushed butchery into a meticulous, sterilized art. A refined and intellectual young man, often seen sporting a mustache and top hat, Halsted indulged in a vibrant social life and possessed an infinite and somewhat untamed curiosity.
With that investigative spirit, Halsted had embarked on experiments with cocaine—then touted as a wonder drug—with a group of colleagues in 1884. Submitting themselves as test subjects, they explored the drug’s pain-numbing abilities by injecting it into their peripheral nerves. In doing so, they would advance the concept of local anesthetic, a critical leap for medical procedures, including dental work. They also became enslaved to the drug, whose dangerously addictive properties were not yet understood. Two of Halsted’s colleagues died within months.
After a string of unexplained absences and erratic behavior at work, Halsted’s close friend William Welch—a pathologist he’d met through New York medical circles—stepped in to lead a series of interventions. The first attempt was rehabilitation by sea, a three-month voyage aboard a schooner to the Windward Islands during which Halsted was supposed to wean himself incrementally from cocaine. By all accounts, the trip was a failure, with a restless Halsted breaking into the captain’s storage to hunt for drugs.
When Halsted returned to land, his family and Welch demanded that he seek treatment at Butler, a well-regarded mental hospital. Welch also dangled encouraging bait for his friend’s recovery: the opportunity to move to Baltimore to help form a new hospital and the nation’s first research university.
For Halsted, this was also a chance to escape the life he’d scorched in New York. Arriving in the new city in December 1886, Halsted joined Welch’s pathology lab while Johns Hopkins Hospital and its medical campus remained under construction.
Shortly after arrival, he relapsed.
Though Halsted’s name has slipped from public prominence in the century since his death, he casts a long shadow at the Johns Hopkins medical campus: in the hospital’s central building named in his honor and in the famous John Singer Sargent painting hanging across the street at the Welch Medical Library, where he’s featured among the institution’s four founding fathers—with Welch, William Osler, and Howard Atwood Kelly.
“He’s been a role model for virtually everyone who has come through Hopkins in the last 100 years to be a surgeon or be trained as one,” says John Cameron, who served as chief of surgery for the hospital for 19 years and has written extensively about Halsted. “He’s really a role model for surgeons all around the world. Many would recognize his name but maybe not know much about him.”
A brilliant, nonconforming, complicated man, Halsted was appointed first surgeon-in-chief of the hospital in 1890 and professor of surgery two years later, at the age of 40.
Despite Halsted’s lifelong battles with addiction, not only cocaine but later morphine, he revolutionized surgery in America by elevating three concepts: anesthesia to control pain, fine instruments to stop bleeding, and antisepsis to prevent infection. One intern observed that the surgeon’s technique was so measured and precise that “there was never a moment of anxiety. I could not believe my eyes. It was like stepping into a new world.”
Halsted had adopted these principles from his post–medical school studies in Austria, Germany, and Switzerland, meccas at the time for doctors in training who had the means to travel. When he returned to New York, he found American physicians puzzlingly reluctant to accept the new knowledge.
“He was one of the first surgeons to employ courtesy in surgery, to show any consideration for the insides of a man he was operating on,” journalist H.L. Mencken wrote in the 1930s. “The old method was to slit a man from the chin down, take out his bowels, and spread them on a towel while you sorted them out. Halsted held that if you touched an intestine with your finger, you injured it, and the patient suffered the effects of the injury.”
Equally significant was the surgical residency program Halsted pioneered at Johns Hopkins, based on the German system he revered. This model—whereby medical school graduates enter university-sponsored, hospital-based training, progressively increasing their responsibilities—endures today across the United States. Halsted’s original trainees replicated the model at other top medical schools, including Harvard, Stanford, and Yale, and from there it proliferated.
This September, members of the Halsted Society, a select group of surgeons from varied fields, are convening in Baltimore to honor the 100th anniversary of the death of their predecessor. “All of us surgeons have a connection to him, in the way we learned our craft,” says Andrew Cameron, who along with his father, John, is a member of the society and today is surgeon-in-chief and professor of surgery at the Johns Hopkins School of Medicine. “Any person who takes a job requiring the public trust, you need real training, and before Halsted there was no system in place for that.”
Halsted’s innovations in the practice of surgery were remarkable. His approach to breast cancer—the “radical mastectomy,” removing not only the breast but also the muscles beneath—was the dominant treatment for decades before modern radiation and chemotherapy. During his New York years, Halsted performed what was possibly the first successful blood transfusion in the U.S.—on his own sister, whom he injected with blood from his arm after finding her unconscious from a postpartum hemorrhage. He later performed the nation’s first gallstone surgery—on his own mother, saving her life through a 2 a.m. operation on her kitchen table.
In an act of chivalry for his future wife, Halsted introduced surgical gloves to the operating room. Caroline Hampton, then Halsted’s chief nurse, found her skin so inflamed by the chemical dip he required before surgery that she threatened to quit. “As she was an unusually efficient woman,” Halsted wrote, “I gave the matter my consideration and one day in New York requested the Goodyear Rubber Company to make, as an experiment, two pairs of thin rubber gloves with gauntlets. On trial these proved to be so satisfactory that additional gloves were ordered.” As one researcher remarked, that might have been the first time the start of a love story was recorded in a medical journal.
William Halsted and Caroline Hampton were both born into privilege and pedigree, their marriage a union of “the wealthy merchant class of the North with the planter aristocracy of the South,” as medical historian Peter Olch wrote. Born in Manhattan on Sept. 23, 1852, Halsted grew up in a grand townhouse on Fifth Avenue, where his family was well established in the dry goods industry and wielded societal influence. He attended the prestigious Phillips Academy in Andover, Massachusetts, then Yale, where he was a middling student but exceptional athlete, captaining the football team. Only as a senior did Halsted’s interest in medicine awaken, when he devoured Gray’s Anatomy and Dalton’s Physiology. He entered the College of Physicians and Surgeons, which would later become Columbia University’s medical school, and graduated among the top 10 of his class in 1877.
Nine years Halsted’s junior, Caroline Hampton was born on Nov. 10, 1861, into the family of famous Confederate General Wade Hampton III, her uncle, and she grew up in the shadow of his ruined Millwood Plantation in Columbia, South Carolina, which Union soldiers burned during the Civil War. Orphaned as a baby, Caroline was raised by three unmarried aunts, and she and her sister attended Edgehill in Virginia, a girls’ school associated with the family of Thomas Jefferson.
In 1885, Hampton made the surprising choice to head to New York City to study nursing. She graduated from New York Hospital three years later before landing the position of chief nurse in the surgical division of the new Johns Hopkins Hospital. “Rather than just trying to follow the conventional life of a Southern belle, she got out of the South … got her diploma and then a job in Baltimore—remarkable achievements for a woman at that time,” says Nancy McCall, director of the Johns Hopkins Chesney Archives.
Independent, aristocratic, and practical in nature, Hampton was by some accounts delightful to friends but perhaps a bit curt and intolerant to others. When frictions arose with another nurse in her unit, Halsted stepped in to appoint Hampton chief nurse of his own operating room.
William Osler, another Johns Hopkins founder, recalled spotting the two flirting, medical-style, in the pathology lab. “One Sunday morning, I … found Dr. Halsted teaching her osteology, demonstrating the fibula. I then knew all that was up with him, and I sat down and chafed him for a few minutes.”
At 37, Halsted broke from bachelorhood and proposed to Hampton in March 1890.
They wed on June 4 that year in Caroline’s world of South Carolina, then honeymooned at the Hampton Lodge in Cashiers, North Carolina—the summer estate of Wade Hampton III, nestled in the Blue Ridge Mountains. The couple returned to this site each summer, ultimately elevating it to the center of their lives. An outdoorswoman and avid rider, Caroline struck a contrast with her citified husband. Later recalling his first trail rides on horseback, William said: “There I was alone in the mountains with this comparatively strange woman, and she wanted me to get off my horse and kill a rattlesnake. She was terribly disgusted when I refused.”
If Caroline was no-nonsense, William was fussy. Known for his elegant fashion, he ordered suits from London and shoes from Paris, where he also mailed some of his dress shirts to be laundered. In the fireplace he would burn only hickory logs aged at least three years. One friend compared the couple to Charles Dickens characters—”so peculiar, eccentric, so unlike other people, yet so interesting doubtless because of their oddities.”
In Baltimore, the Halsteds settled into a stone house at 1201 Eutaw Place, crowding it with antiques, books, and knickknacks. Childless, they kept company with dogs, most memorably a pair of dachshunds named Nip and Tuck. In an arrangement not unusual during Victorian times, Hampton occupied the third floor and Halsted the second, and the two would join each evening for dinner, chatting about “everything from the origin of words to the origins of man, farming, forestry, etc.,” as Caroline once said. The bond between the couple was intellectual, and though Caroline left nursing after her wedding, she is thought to have had “a powerful effect on Halsted’s career,” as Mencken said. “Many of the Halsted techniques for surgery were due to her suggestions.”
Undoubtedly, the two were most content in their remote mountain sanctuary, High Hampton, where they spent progressively more time as the years passed. After their honeymoon there, William had purchased the 450-acre property from Hampton’s aunts, adding to it over time. They built a pinewood cottage surrounded by fields, streams, and forests and kept a stable of cattle and horses.
Removed from society, William and Caroline savored their reclusiveness and flourished in their hobbies. Caroline was known to rise at dawn, put on a pair of sturdy boots, then set to gardening, farming, and tending the animals. William developed a passion for astronomy and for growing dahlias. His garden, in fact, became one of the greatest dahlia collections in the country, and a form of it survives today on the land.
In the spring of 1922, the National Dental Association honored Halsted for his pioneering work with local anesthetic—the positive result of his otherwise disastrous experiments with cocaine. Halsted must have had mixed emotions that evening, at the banquet at Baltimore’s Belvedere Hotel. He later told a friend that his happiness was “tinged with regret for the lost opportunities—for the time wasted from loss of health”— seemingly acknowledging the damage cocaine had wrought.
In those early experiments with the white powder, Halsted was truly working at the cutting edge of medicine. Although cocaine was a common and perfectly legal ingredient in tonics and eventually the famous Coca-Cola, its medical potential was unappreciated and undocumented until 1884. That year, famed Austrian psychoanalyst Sigmund Freud published “Über Coca,” the first scientific analysis of cocaine, and his colleague, ophthalmologist Carl Koller, followed with a seminal paper heralding the drug’s promise as an anesthetic for eye surgery.
Across the Atlantic, Halsted took note, ordering a bulk supply of cocaine within weeks of Koller’s report. Despite the wealth of data the surgeon accumulated from his investigations, he published only one paper on the topic, a notorious 1885 entry in the New York Medical Journal whose rambling incoherence suggests he was high while writing.
With the perspective of time, Halsted’s life can be understood in two distinct phases: before cocaine and after. The energetic, affable man he was in New York—socializing and entertaining often, highly engaged with students—was not the Halsted people knew later in Baltimore, a withdrawn, wary, and enigmatic figure. His friend Harvey Cushing described him as “caring little for the gregarious gatherings of men.” According to Welch, Halsted could still be charming with close friends, “full of original, whimsical humor,” but he often failed to restrain his “caustic irony” at inappropriate times.
In the phase in between, Halsted completed two separate stints rehabilitating at Butler, which together consumed more than a year of his life. Many believe that his treatment there to ease cocaine withdrawal included daily injections of morphine—in effect, trading one highly addictive drug for another.
The morphine addiction haunted Halsted throughout his life. Although it was the subject of whispers around Johns Hopkins, he guarded his secret from all but a few intimates, including Welch and Osler. In the Inner History of Johns Hopkins Hospital, Osler recalled finding Halsted, the newly appointed surgeon-in-chief, “in a severe chill” one day. “[T]his was the first intimation I had that he was still taking morphine,” Osler wrote. “Subsequently we had many talks, and I gained his full confidence. He had never been able to reduce the amount to less than three grains daily; on this he could do his work comfortably and maintain his excellent physical vigor.” (For context, that dosage is equivalent to 195 milligrams, while modern pain treatment calls for just 10 to 20 milligrams every four hours.)
Caroline certainly knew of her husband’s addiction, but it’s not clear how she coped with it—and Daniel Nunn, former historian for the Halsted Society, found anecdotal evidence that morphine may have hooked her too. One caretaker recalled her becoming “very upset because a package had not arrived from Parke-Davis”—a pharmaceutical company that sold the drug.
In an otherwise storied career, Halsted was notorious for spotty attendance and prolonged absences that would have ended the employment of a lesser surgeon. Meeting notes from the hospital’s board of trustees express frustration and concern. “We have much troubled over Halsted,” says one 1891 note. “He went to South Carolina a month ago for his health and will not be back until the middle of the month. He was looking dreadfully when he left.”
In the days leading to his death, in the summer of 1922, Halsted relied on constant use of morphine to treat his escalating pain, as gallstones in his liver caused nausea, fever, vomiting, and jaundice. As his condition worsened, he ended his vacation in High Hampton early to be admitted to Johns Hopkins Hospital.
Strikingly, Halsted’s death featured a mix of elements that also defined his life, notes Ralph Hruban, professor of oncology and pathology at the Johns Hopkins School of Medicine, who produced a PBS documentary on Halsted in 2011. Halsted died at his own workplace, under the care of two chief residents he had trained himself. “The irony is, Halsted performed the first gallstone operation and the first blood transfusion—then what does he die from? Gallstones. And one of the residents sticks a needle in his own vein to give Halsted his blood,” Hruban says.
Despite the efforts of his former students, Halsted succumbed to post-operative infection on Sept. 7, 1922, just shy of his 70th birthday. Caroline survived her husband by a mere three months. Deep in grief, she died of pneumonia on Nov. 27, 1922.
In death, William and Caroline returned to their roots. William’s headstone stands in Greenwood Cemetery in Brooklyn, New York, among his family, and Caroline is buried among her own kin more than 700 miles south, at the church where she and Halsted wed. In his will, Halsted bequeathed his Baltimore property and his possessions to Johns Hopkins, where many artifacts remain in the archives today, including his spectacles, his operating table, and his signature top hat.
If William Halsted were alive today, he would surely wince in shame that his legacy as the father of modern surgery is so intertwined with the addictions he sought to keep private. But as John Cameron says, it’s an integral part of the story. If not for his cocaine addiction, Halsted probably wouldn’t have accepted Welch’s invitation to Baltimore. “An unusual set of circumstances led Halsted to Baltimore and Johns Hopkins Hospital, and the result was an amazing productivity that led to the creation of our surgical heritage,” Cameron wrote in one article.
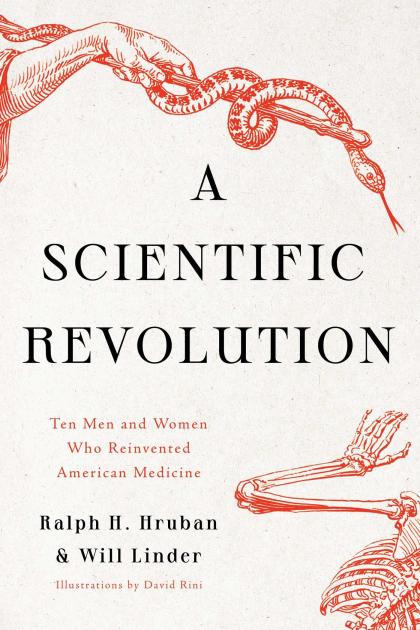
Moreover, Halsted’s accomplishments at Johns Hopkins seem all the more remarkable considering he was wrestling with morphine the entire time. “He never overcame it. He lived with it. And yet he achieved more than most people, and here we are still talking about him,” says Hruban, who profiled Halsted in the new book he co-authored with Will Linder, A Scientific Revolution: Ten Men and Women Who Reinvented American Medicine.
Today, the medical principles that Halsted advanced are taken for granted. But 100 years past his death, his mark is still there—every time a dentist numbs a mouth, every time a doctor or nurse gloves up, every time a gallstone is removed or blood transfused. Every time a patient lies on the operating table, succumbing to the fog of anesthesia, fading into the trust of a surgeon.
Katie Pearce is a senior writer for Johns Hopkins Magazine.
Review By: JoAnn Greco / Published Fall 2022 / Johns Hopkins Magazine
The characters profiled in A Scientific Revolution: Ten Men and Women Who Reinvented American Medicine (Pegasus Books, 2022) by Ralph H. Hruban, Med ’85, and Will Linder, A&S ’72, sure would make for one fascinating fantasy dinner party. There’s the no-BS woman who helped stir the Johns Hopkins School of Medicine to life, the white men who cemented its reputation, and the Black technician who worked patiently—and in relative obscurity—for decades alongside one of its groundbreaking surgeons.
The authors kick off their profiles of 10 of the school’s iconoclasts with the indomitable Mary Elizabeth Garrett, a railroad heiress and feminist philanthropist who convinced Johns Hopkins leadership to admit women to its new School of Medicine as a condition of her donating the necessary funding for it to open in 1893.
Four of the next concise but richly detailed portraits bring to life the innovative and risk-taking physicians who flourished during the school’s early days. We have William Henry Welch, its first dean, and William Osler, who brought students into patient wards and published the field’s definitive medical textbook (The Principles and Practice of Medicine). A pair of derrring-doers, the surgeon William Stewart Halsted (who once jabbed a syringe into himself to perform an impromptu blood transfusion) and Jesse William Lazear (whose explorations of infectious diseases included an ultimately deadly exposure to yellow fever-infected mosquitoes) completes this quartet of willful Williams.
Two other nonmedical personalities flesh out the development of the school. The multitalented Civil War veteran John Shaw Billings combined his affinity for what today might be referred to as information management and environmental design to bring light, air, and organization into Hopkins’ medical facilities. The German-born Max Brödel revolutionized the art of anatomical illustration. In a nod to that legacy, David Rini, a professor in the Department of Art as Applied to Medicine, for which Brödel served as the first director, drew the expressive character portraits that open each chapter.
Wary of hagiography, the authors take pains to address the less savory aspects of, say, Brödel (racist attitudes) and Halsted (drug addiction). They also acknowledge the institution’s susceptibility to contemporary prejudices.
Dorothy Reed Mendenhall, who identified the cellular components of Hodgkin lymphoma, surmounted a life beset by tragedy. As a 6-year-old, she experienced the sudden death of her father; as a young married woman she endured the deaths of her first two children. Her battle against sexism started early, too: on her first day of medical school, Osler sidled up to her and hissed “go home.” Helen Taussig and Vivien Thomas, a white female doctor and a Black male surgical technician, also fell prey to the era’s sexism and racism and were routinely overshadowed by the pioneering heart surgeon who performed the lifesaving blue baby surgery they had conceived of and perfected. Still, they persisted. And that, suggest the authors, is the heart of science and the heart of Hopkins.
For more information on the book and its central figures, we reached out to author and alum Ralph Hruban, a professor of pathology and oncology, who, in the early days of the pandemic, delivered a series of virtual talks highlighting some of the pivotal figures in the history of the Johns Hopkins School of Medicine.
How did you and your co-author Will Linder come together and what were your roles in writing the book?
Will was sitting in on the lectures and reached out to me later about expanding them into a book. It was a wonderful match. I love the 50,000-foot view and telling stories, and Will is a skilled writer with an eye for evocative detail. We started with the standard texts on our subjects then accessed several online archives. I also spent a lot of time at [Hopkins’] Chesney Archives. We came across some real eye-openers, like the original manuscript for Vivien Thomas’ autobiography. We compared it line for line with the published version, which effectively put to rest the suspicions that some had about whether a Black man with no college education could have written the book himself.
Besides your affiliations, what drove you to focus on Hopkins?
There was an inflection point in the history of medicine in the United States that starts with the opening of Hopkins’ School of Medicine and continues through 1910 with the release of the Flexner Report. That report basically said that American medical education was a mess, and everyone was doing it wrong except Hopkins. It resulted in the closing of the fee-for-service medical schools and commitments to invest in schools modeled on Hopkins.
Some of the figures you profile are famous, some not. What were your criteria for inclusion?
Mostly, we were looking for narrative arcs. Florence Sabin [the first woman to hold a professorship at the School of Medicine] deserved the full treatment, but her story wasn’t as compelling, so we just touch upon her here and there. Then there’s someone like Billings, who’s kind of underappreciated. What an amazing career he had. I love that his idea for a punch card system ended up as the foundation for a company that later became IBM!
Did anyone emerge as a personal favorite?
My admiration for Taussig kept growing. I love the anecdote about her trainees commissioning a portrait from Jamie Wyeth on her retirement. He met her in Cape Cod, he had dinner with her and walked on the beach with her, and he was so impressed by her forthright stare and how she didn’t care about her appearance. Well, people cried when the painting was unveiled, and after she died, they asked the school to burn it. Will and I both love her and the painting.
Can you recall any surprises or uncomfortable truths that you discovered?
The new scholarship about Osler’s racial prejudices is certainly disappointing. But I think his comments just reveal that we’re all human and that even someone so well regarded can have their own unconscious biases. The writing process for me revealed some of my own biases. For example, the implicit sexism in a line from Reed’s principal biographer didn’t even occur to me as perpetuating gender stereotypes until my wife pointed it out! [The passage, from an article written in 2003, characterizes Reed’s affair with a rising star in the Pathology Department this way: “She gave him her heart, and in return he gave her international fame.”]